When to Call the Doctor for Your Newborn Baby: A Complete Guide for New Parents
As new parents, one of the most anxiety-inducing aspects of caring for a newborn is knowing when something is truly wrong and when symptoms are normal parts of infant development. Every cough, unusual cry, or change in feeding pattern can send parents into a spiral of worry. At myPediaClinic Dubai, we understand these concerns and want to empower you with the knowledge to distinguish between situations that require immediate medical attention and those that can wait for a routine visit. This comprehensive guide will help you recognize warning signs in newborns, understand when to seek urgent care, and feel confident in your ability to care for your baby’s health.
Emergency Warning Signs – Call 999 or Go to Emergency Immediately
- Difficulty breathing, rapid breathing, or pauses in breathing lasting more than 10 seconds
- Blue or gray color around the lips, tongue, or face
- Unresponsive or extremely difficult to wake
- Seizures or convulsions
- Temperature above 38°C (100.4°F) in babies under 3 months
- Signs of severe dehydration (no wet diapers for 6+ hours, no tears when crying, sunken soft spot)
- Projectile vomiting repeatedly
- Blood in vomit, stool, or urine
Understanding Newborn Health: What’s Normal and What’s Not
The first few weeks with a newborn involve countless new experiences and observations that can be confusing for even the most prepared parents. Newborns have many behaviors and physical characteristics that may seem alarming but are actually completely normal. Understanding these normal variations helps you focus your concern on situations that truly require medical attention.
At myPediaClinic, our pediatricians regularly reassure new parents about common newborn behaviors. Hiccups, sneezing, irregular breathing patterns during sleep, and startling reflexes are all normal newborn behaviors that don’t require medical intervention. Similarly, crossed eyes, mild acne, and dry or peeling skin are typical in the first weeks of life.
However, distinguishing normal from concerning requires careful observation and knowledge. The key is learning to recognize patterns and changes from your baby’s baseline behavior. A symptom that might be normal for one baby could be concerning for another, which is why establishing a relationship with a trusted pediatrician is so important during your baby’s early weeks.
Fever in Newborns: A Critical Warning Sign
Fever in a newborn is taken very seriously by medical professionals because young babies have immature immune systems and limited ability to fight infections. What might be a minor illness in an older child could be a serious infection in a newborn, making fever one of the most important warning signs to recognize and act upon quickly.
When Fever Requires Immediate Medical Care
Any baby under three months old with a rectal temperature of 38°C (100.4°F) or higher should be seen by a doctor immediately, regardless of how the baby appears otherwise. This is not a situation to wait and see or to try to manage at home. Even if your baby seems relatively well, fever at this age requires prompt medical evaluation to rule out serious bacterial infections.
The reason for this urgency is that newborns and young infants can have serious infections without showing typical signs of illness. Their immune systems respond differently than those of older children and adults, meaning they can deteriorate quickly. At myPediaClinic Dubai, we have protocols in place for rapid evaluation of febrile infants because we understand the importance of quick assessment and treatment.
How to Properly Check Your Baby’s Temperature
Rectal temperature is the most accurate method for measuring a newborn’s temperature and is the standard used in medical settings. To take a rectal temperature, use a digital thermometer with a flexible tip, apply a small amount of petroleum jelly to the tip, gently insert about half an inch into your baby’s rectum, and hold in place until the thermometer signals it’s done.
Avoid using forehead strips, ear thermometers, or armpit readings for newborns, as these methods are less accurate in young babies. If your baby feels warm to the touch and you don’t have a thermometer available, contact your pediatrician for guidance. Never give fever-reducing medication to a newborn without first consulting your doctor.
What to Expect at the Doctor for Newborn Fever
When you bring a febrile newborn to the doctor or emergency room, expect a thorough evaluation. This typically includes a complete physical examination, blood tests to check for infection markers, urine analysis, and possibly a spinal tap (lumbar puncture) to check for meningitis. While these tests may seem scary, they are essential to ensure any serious infection is identified and treated promptly.
Breathing Problems: When to Be Concerned
Newborns breathe differently than older children and adults, and understanding normal newborn breathing patterns helps you recognize when something is wrong. Normal newborn breathing can be irregular, with occasional pauses and periods of faster breathing, especially during sleep. However, certain breathing patterns indicate respiratory distress and require immediate medical attention.
Normal Newborn Breathing Patterns
Healthy newborns typically breathe 30-60 times per minute, which may seem rapid compared to adult breathing. During sleep, it’s normal for newborns to have periodic breathing, where they breathe rapidly for a few seconds, then pause briefly, then breathe rapidly again. Brief pauses of up to 10 seconds are generally not concerning if the baby’s color remains normal and they resume breathing on their own.
Newborns are obligate nose breathers for the first several months, meaning they breathe primarily through their noses. This can cause noisy breathing when nasal passages are congested, which is common due to narrow nasal passages and increased mucus production. Occasional snorts, grunts, and squeaks during sleep are usually normal.
Signs of Respiratory Distress Requiring Medical Care
Seek immediate medical care if your newborn shows any of these signs:
- Breathing rate consistently above 60 breaths per minute
- Grunting sound with each breath
- Flaring nostrils with breathing
- Retractions (skin pulling in between ribs, below ribs, or above collarbones)
- Blue or purple color around lips, tongue, or nails
- Pauses in breathing lasting more than 10 seconds
- Unusual lethargy or difficulty waking
- Refusal to feed due to difficulty breathing
These signs can indicate various conditions ranging from respiratory infections to heart problems. Prompt evaluation by a pediatric specialist is essential to determine the cause and begin appropriate treatment. Trust your instincts; if your baby’s breathing looks or sounds unusual to you, it’s always better to have them evaluated.
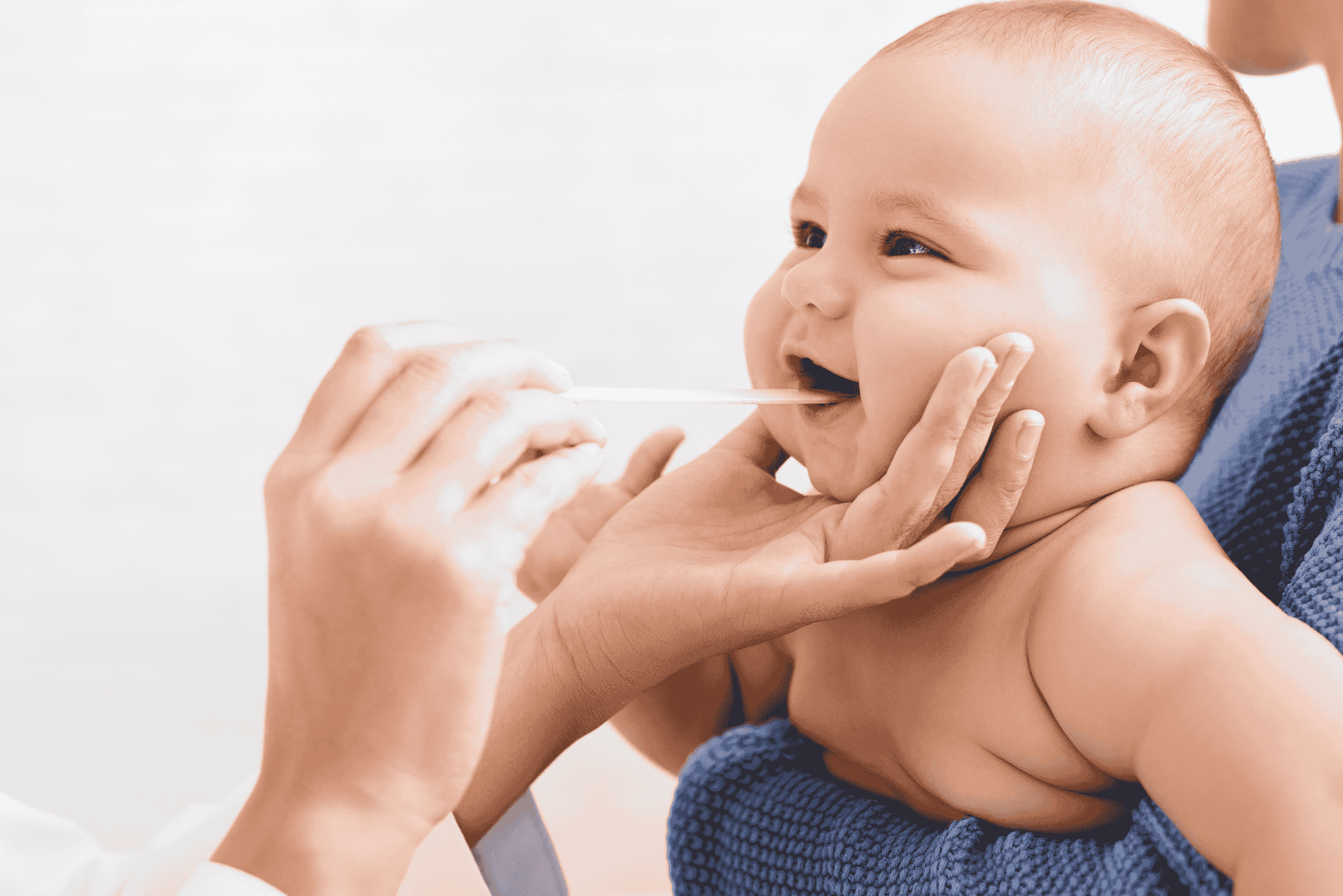
Feeding Concerns: When Eating Problems Signal Trouble
Feeding is one of the most important activities for a newborn, providing essential nutrition for growth and development. Changes in feeding patterns can be one of the earliest signs that something is wrong with your baby. Understanding normal feeding patterns and recognizing concerning changes helps you know when to seek medical advice.
Normal Newborn Feeding Patterns
Newborns typically feed 8-12 times in 24 hours, or roughly every 2-3 hours. Breastfed babies may feed more frequently because breast milk is digested more quickly than formula. During growth spurts, babies may want to feed even more often, which is normal and helps increase milk supply for breastfeeding mothers.
It’s normal for newborns to be sleepy feeders, especially in the first week or two of life. Some babies need to be awakened and encouraged to feed during this period. After the first few weeks, most babies become more alert and feed more efficiently, with feeding sessions typically lasting 10-20 minutes on each breast or about 15-30 minutes for bottle feeding.
When to Call the Doctor About Feeding
Contact your pediatrician if your newborn shows any of the following feeding-related concerns:
- Refuses to feed or shows decreased interest in feeding for more than 6-8 hours
- Consistently takes less than the expected amount at most feedings
- Appears too weak or tired to complete feedings
- Has difficulty latching or sucking effectively
- Consistently vomits large amounts after feedings (not just spit-up)
- Shows signs of dehydration (fewer than 6 wet diapers per day after day 5)
- Loses more than 10% of birth weight or doesn’t regain birth weight by 2 weeks
Feeding difficulties can indicate various issues, from minor problems like a tight frenulum (tongue-tie) to more serious conditions like infections or heart problems. Early intervention for feeding issues is important to ensure your baby is receiving adequate nutrition for healthy growth and development.
Understanding Spit-Up vs. Vomiting
Spit-up is common in newborns and is usually not concerning. It typically occurs shortly after feeding, involves a small amount of milk, and the baby seems comfortable and content. Most babies spit up at least occasionally, and some spit up with nearly every feeding while still gaining weight normally.
Vomiting is different from spit-up and can be concerning in newborns. Warning signs include: forceful or projectile vomiting, vomit that is green or yellow (bile-stained), blood or dark brown material in vomit, vomiting accompanied by fever or lethargy, and repeated vomiting episodes. Any of these signs warrant a call to your doctor or a visit to myPediaClinic.
Jaundice: When Yellow Skin Needs Medical Attention
Jaundice, the yellowing of the skin and eyes caused by elevated bilirubin levels, is very common in newborns. Mild jaundice typically appears on day 2-3 of life, peaks around day 5, and resolves on its own within 2 weeks. However, severe jaundice or jaundice that persists requires medical evaluation and treatment to prevent complications.
Monitoring Jaundice at Home
Check your baby for jaundice in natural daylight by gently pressing on your baby’s nose or forehead; the skin should look yellow before returning to its normal color if jaundice is present. Jaundice typically starts on the face and progresses downward to the chest, abdomen, and legs as bilirubin levels increase.
Normal physiological jaundice improves gradually, with the yellow color fading from the legs upward as bilirubin levels decrease. Good feeding helps clear bilirubin from your baby’s system, so ensuring your baby is feeding well and having regular bowel movements is important.
When Jaundice Requires Medical Attention
Call your doctor or seek immediate care if:
- Jaundice appears within the first 24 hours of life
- Yellow color spreads to arms, legs, or abdomen
- Jaundice becomes deeper or more pronounced
- Your baby is difficult to wake or unusually lethargic
- Your baby is not feeding well
- Jaundice persists beyond 2 weeks
- Your baby has pale stools or dark urine
- You notice high-pitched crying or unusual irritability
Severe jaundice that is not treated can lead to kernicterus, a form of brain damage. The pediatricians at myPediaClinic routinely screen for jaundice and can advise when treatment such as phototherapy is needed.
Skin Changes and Rashes: What to Watch For
Newborn skin goes through many changes in the first weeks of life, and most skin conditions in newborns are benign and resolve on their own. However, certain skin changes can indicate infection or other problems requiring medical attention.
Normal Newborn Skin Changes
Many skin conditions in newborns are completely normal and require no treatment:
- Erythema toxicum: Red blotchy patches with small white or yellow bumps that come and go
- Milia: Tiny white bumps on the nose and face
- Baby acne: Small red bumps on the face appearing around 2-4 weeks
- Cradle cap: Scaly, crusty patches on the scalp
- Peeling skin: Especially common in post-term babies
- Mongolian spots: Bluish-gray patches on the back or buttocks
- Stork bites: Pink or red marks on the eyelids, forehead, or back of neck
Skin Changes Requiring Medical Attention
Contact your pediatrician if you notice:
- Rash with fever
- Blisters or fluid-filled bumps
- Rash that looks like bruises or blood spots under the skin
- Spreading redness around the umbilical cord stump
- Pus or foul-smelling discharge from any area
- Yellowing of the skin (jaundice)
- Any rash that seems to be spreading or worsening
Umbilical Cord Care and Concerns
The umbilical cord stump typically falls off between 1-3 weeks after birth. During this time, proper care and monitoring for signs of infection are important. Most cord issues are minor, but certain signs require prompt medical attention.
Normal Umbilical Cord Changes
As the cord stump dries and heals, it changes from yellowish-green to brown to black before falling off. A small amount of discharge or dried blood around the base is normal. After the stump falls off, you may notice a small raw area that heals within a few days.
Signs of Umbilical Cord Infection (Omphalitis)
Seek medical care immediately if you notice:
- Red, swollen skin spreading from the cord base
- Pus or foul-smelling discharge
- Bleeding that won’t stop with gentle pressure
- Fever
- Baby seems irritable or unwell
Umbilical cord infection can become serious quickly in newborns, so any signs of infection should be evaluated promptly by a healthcare provider.
Bowel Movements and Urination: Monitoring Output
Tracking your newborn’s diaper output is an important way to ensure they are feeding adequately and staying hydrated. Changes in bowel movement patterns or decreased urine output can indicate feeding problems or illness.
Normal Newborn Diaper Output
In the first few days of life, babies have meconium stools (dark, tarry bowel movements) that transition to yellow, seedy stools for breastfed babies or tan, firmer stools for formula-fed babies. By day 4-5, babies should have at least 3-4 stools per day, though some breastfed babies may stool with every feeding.
For urination, expect at least one wet diaper on day 1, two on day 2, and increasing until your baby has at least six wet diapers per day by day 5. Urine should be pale yellow; dark or concentrated urine may indicate dehydration.
When to Call the Doctor About Diaper Output
Contact your pediatrician if:
- Your baby has fewer than 6 wet diapers per day after day 5
- Stools are white, gray, or pale
- Blood is present in stools or urine
- No bowel movement for more than 4-5 days (after the first week)
- Stools are extremely watery or explosive
- You notice orange or brick-colored spots in the diaper (may indicate concentrated urine)
Crying and Behavior Changes
Newborns communicate primarily through crying, and learning to interpret your baby’s cries takes time. While crying is normal and expected, certain types of crying or behavioral changes can indicate that something is wrong.
Normal Newborn Crying
Healthy newborns typically cry 2-3 hours per day, often more in the evening. Common reasons for crying include hunger, need for a diaper change, tiredness, overstimulation, or simply wanting to be held. Many babies have a fussy period in the late afternoon or evening that is not related to any particular need.
Concerning Crying Patterns
Call your doctor if your baby:
- Has a weak, whimpering cry or unusually high-pitched cry
- Cries inconsolably for more than 3 hours
- Has sudden changes in cry pattern or intensity
- Cries when touched or moved in a way they previously tolerated
- Is unusually quiet or unresponsive
- Cannot be consoled by normal soothing methods
Changes in Alertness and Activity
Newborns sleep 16-17 hours per day in the first weeks, waking primarily for feeding. While sleepy newborns are normal, a baby who is difficult to wake for feedings, appears limp or floppy, or has decreased movement compared to their usual activity may be ill and should be evaluated promptly.
Similarly, unusual irritability where your baby seems uncomfortable regardless of what you try, excessive jitteriness, or inconsolable crying can indicate illness or discomfort that requires medical evaluation.
Eye Problems in Newborns
Newborn eyes often have minor issues that resolve on their own, but certain eye symptoms require medical attention to prevent complications or identify underlying conditions.
Normal Newborn Eye Characteristics
It’s normal for newborns to have occasional crossed eyes, as their eye muscles are still developing coordination. Mild swelling or redness immediately after birth typically resolves within days. Small amounts of white or yellow discharge, especially in the inner corners, are common due to blocked tear ducts.
Eye Symptoms Requiring Medical Attention
Contact your pediatrician if you notice:
- Persistent swelling, redness, or significant discharge
- Eyes that are constantly crossed after 3 months of age
- Thick yellow or green discharge
- Red or bloodshot appearance of the white part of the eye
- Crusting that prevents the eye from opening
- Cloudiness or white spots on the pupil
- Unusual sensitivity to light
When to Schedule Routine vs. Urgent Appointments
Understanding the difference between situations that need routine attention and those requiring urgent care helps you respond appropriately to your baby’s health concerns.
Can Wait for Regular Office Hours
- Minor skin rashes without fever
- Mild congestion without difficulty breathing
- Questions about feeding amounts or schedule
- Minor spit-up concerns
- Baby acne or cradle cap
- Questions about normal newborn behavior
Call Your Pediatrician Today
- Fever in a baby 3 months or older
- Persistent crying lasting several hours
- Changes in feeding patterns
- Rash that is spreading
- Signs of possible ear infection
- Concerns about weight gain or dehydration
- Any symptoms that worry you
Seek Immediate Medical Care
- Fever in any baby under 3 months
- Difficulty breathing
- Blue or gray color
- Seizures
- Unresponsiveness
- Signs of severe dehydration
- Blood in vomit or stool
- Projectile vomiting
Building a Relationship with Your Pediatrician
Having a trusted pediatrician is one of the most valuable resources for new parents. Your pediatrician knows your baby’s individual health history and can provide personalized guidance for your specific concerns.
Well-Baby Visits in the First Months
Regular well-baby visits are scheduled at specific intervals during your baby’s first year, typically at 2-3 days after hospital discharge, 2 weeks, 1 month, 2 months, 4 months, 6 months, 9 months, and 12 months. These visits allow your pediatrician to monitor growth and development, address your questions and concerns, and provide preventive care including vaccinations.
At myPediaClinic Dubai, we encourage parents to come prepared with questions and observations for each well-baby visit. No question is too small or silly when it comes to your baby’s health.
When in Doubt, Call
If you’re unsure whether your baby’s symptoms warrant a call to the doctor, it’s always better to call and ask. Experienced pediatricians and nurses can help you assess symptoms over the phone and advise whether your baby needs to be seen. Trust your instincts as a parent; you know your baby better than anyone, and if something seems wrong, it’s worth getting checked.
Preparing for Emergencies
While we hope you never need to use it, being prepared for medical emergencies gives you peace of mind and ensures you can act quickly if needed.
Information to Have Ready
Keep this information easily accessible:
- Your pediatrician’s phone number and after-hours contact
- Nearest emergency room location
- Poison control center number
- Your baby’s birth date and weight
- Any known allergies or medical conditions
- Medications your baby takes
Infant First Aid and CPR
Consider taking an infant CPR and first aid course before your baby arrives or in the early weeks after birth. Knowing how to respond to choking, breathing emergencies, and other urgent situations can be life-saving. Many hospitals and community organizations offer these courses specifically for new parents.
Frequently Asked Questions About Newborn Health Concerns
A rectal temperature of 38°C (100.4°F) or higher is considered a fever in a newborn. For babies under 3 months old, any fever is a medical emergency that requires immediate evaluation. Use a rectal thermometer for the most accurate reading in newborns.
In the first few days, expect about one wet diaper per day of life (one on day 1, two on day 2, etc.). By day 5-6, your baby should have at least 6 wet diapers per day. Fewer wet diapers can indicate dehydration or inadequate feeding and should be discussed with your pediatrician.
Brief pauses in breathing (up to 10 seconds) during sleep are normal in newborns and are called periodic breathing. However, pauses longer than 10 seconds, breathing that causes color changes, or breathing accompanied by grunting, flaring nostrils, or chest retractions require immediate medical attention.
Seek medical attention if jaundice appears within 24 hours of birth, spreads to arms and legs, becomes more intense, persists beyond 2 weeks, or is accompanied by poor feeding, lethargy, high-pitched crying, or pale stools. Mild jaundice appearing on day 2-3 and resolving by 2 weeks is usually normal.
Signs of dehydration in newborns include fewer than 6 wet diapers per day (after day 5), dark concentrated urine, no tears when crying, dry mouth, sunken soft spot (fontanelle) on top of the head, lethargy, and poor feeding. Dehydration can become serious quickly in newborns and requires prompt medical attention.
Spit-up (a small amount of milk coming up) is normal and common in newborns. However, vomiting (forceful expulsion of larger amounts) can be concerning. Seek medical care if vomiting is projectile, contains blood or green/yellow bile, occurs repeatedly, or is accompanied by fever, lethargy, or signs of pain.
Signs of umbilical cord infection include redness spreading from the base, foul-smelling discharge, pus, bleeding that won’t stop, and fever. If you notice any of these signs, contact your pediatrician immediately, as umbilical cord infections can become serious quickly in newborns.
Newborns typically cry 2-3 hours per day, which is normal. However, call your doctor if crying is inconsolable for more than 3 hours, the cry sounds unusually weak or high-pitched, your baby seems in pain, or the crying pattern changes significantly from what’s normal for your baby.
In the first few weeks, yes. Newborns need to feed every 2-3 hours to gain weight and stay hydrated. If your baby consistently sleeps through feeding times and is difficult to wake, seems unusually lethargic, or isn’t producing enough wet diapers, contact your pediatrician as this could indicate illness.
Your newborn should see a pediatrician within 2-3 days after leaving the hospital, especially for breastfed babies to ensure feeding is going well. This early visit checks for jaundice, monitors weight, and addresses any concerns. Subsequent well-baby visits are typically at 2 weeks, 1 month, and then every 1-2 months in the first year.
Expert Pediatric Care for Your Newborn in Dubai
Your newborn’s health is precious, and having access to trusted pediatric care gives you peace of mind during the beautiful but sometimes anxious early weeks of parenthood. At myPediaClinic Dubai, our experienced pediatric team is here to support your family with compassionate, expert care for all your newborn’s health needs, from routine well-baby visits to urgent concerns.